
- #Postpartum retained placental fragments defined manual#
- #Postpartum retained placental fragments defined trial#
However, the vast preponderance of normal over prolonged third stages may have skewed the correlation analysis of blood loss over time, thus weakening the argument for early MROP, an invasive and potentially unnecessary procedure with attendant risks. Evidence favoring MROP within 30 min, based on increasing PPH risk with the duration of the third stage of labor, emerged from studies combining women with normal and prolonged third stages.
#Postpartum retained placental fragments defined manual#
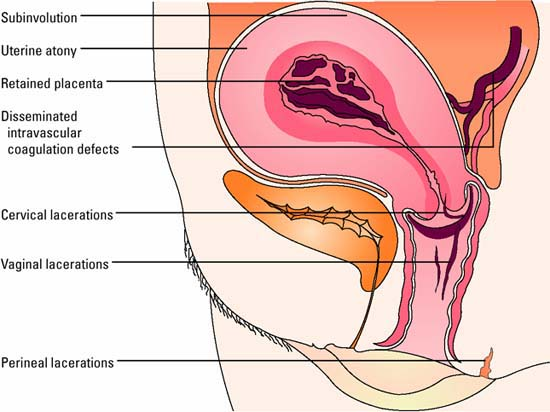
ĭivergence persists over the optimal timing for manual removal of the placenta (MROP): ≥ 60 min in Northern Europe vs ≤ 30 min in Central and Southern Europe. 90% of placentas deliver spontaneously within 15 min (9 min in active management ) only 2.2% remain undelivered at 30 min. Expulsion is rapid after vaginal delivery. Prevalence is higher in high- vs low-income countries (2.7% vs 1.5%). A placenta is deemed retained if not expelled within 30 min postpartum. The third stage of labor starts after the delivery of the child and ends with the delivery of the placenta. Etiologies include uterine atony, cervical or vaginal laceration, coagulopathy, and in 19.8% of cases retained placenta. Postpartum hemorrhage (PPH) is the leading cause of maternal mortality worldwide: in 2003–2009, hemorrhage accounted for 27.1% of maternal deaths, over two-thirds of which were classified as PPH.
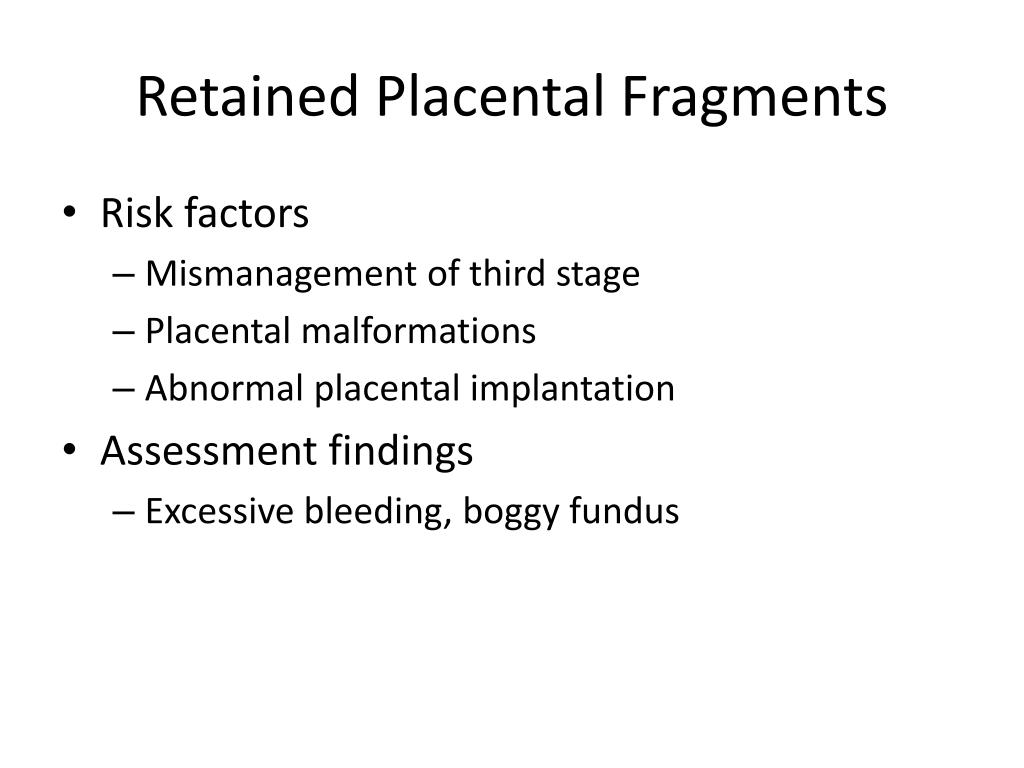
The prompt detection of uterine atony and immediate prerequisites for manual removal of the placenta are key factors in the management of postpartum hemorrhage. Our results suggest that there is neither a safe time window preceding postpartum hemorrhage, nor justification for an early cut-off for manual removal of the placenta. Postpartum blood loss does not correlate with third stage duration in women with retained placenta. Uterine atony was significantly associated with greater decrease in hemoglobin ( p < 0.001), higher measured blood loss ( p < 0.001), postpartum hemorrhage ( p = 0.048), and need for blood transfusion ( p < 0.001).
A shorter third stage (< 60 min) was associated with significantly increased uterine atony ( p = 0.001) and need for blood transfusion ( p = 0.006). ResultsĬorrelation analysis revealed no association between third stage duration and measured blood loss or decrease in hemoglobin. We evaluated the relationship between these two blood loss parameters and the duration of the third stage of labor using Spearman rank correlation, followed by subgroup analysis stratified by third stage duration and retained placenta etiology. Blood loss was measured using a validated and accurate technique based on calibrated blood collection bags, backed by the post- vs pre-partum decrease in hemoglobin. Our retrospective study analyzed a single-center cohort of 296 women with retained placenta. We investigated the influence of the time factor and retained placenta etiology on postpartum hemorrhage dynamics. Retained placenta accounts for nearly 20% of severe cases. Ander D Weeks (2001) The Retained Placenta.Postpartum hemorrhage is the major cause of maternal mortality worldwide.(2017) The inherited risk of retained placenta: A population based cohort study. Ander D Weeks (2008) The retained placenta.(2009) Factors associated with peripartum hysterectomy.
#Postpartum retained placental fragments defined trial#


 0 kommentar(er)
0 kommentar(er)
